Abstract

Background: Anticoagulation for 3-6 months is the minimum required duration of treatment for patients with venous thromboembolism (VTE). Whether to extend treatment beyond the initial 3-6 months of anticoagulation in patients with a first unprovoked VTE has been debated. The American Society of Hematology guidelines suggest continuing anticoagulation indefinitely over discontinuing anticoagulation after completing 3-6 months of initial treatment for a first unprovoked VTE, except in patients who have a high risk for bleeding (Ortel T, Blood Adv 2018). However, the lifetime clinical benefits, harms, and cost-effectiveness of indefinite anticoagulation have not been formally assessed. While a randomized controlled trial (RCT) would be the optimal study design to provide evidence for or against continuing anticoagulation indefinitely in patients with a first unprovoked VTE, it is unlikely to be conducted due to the lifelong (i.e. until death) follow-up and extremely large sample size that would be required.Decision-analytic modelling can provide evidence to inform guidelines under circumstances in which RCTs are unfeasible.
Objective: The aim of this modelling study was to compare the clinical benefits, harms, and cost-effectiveness of continuing versus discontinuing anticoagulation indefinitely after completing initial treatment for a first unprovoked VTE.
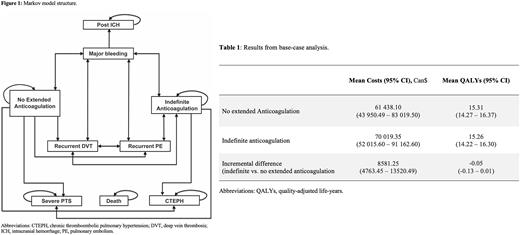
Methods: We created a probabilistic Markov cohort simulation model [Figure 1] to simulate costs (adjusted to 2022 Canadian dollars) and outcomes (recurrent VTE, major bleeding, and quality-adjusted life-years [QALYs]) for two hypothetical cohorts of patients aged 55 years with a first unprovoked VTE that had completed 3-6 months of initial anticoagulant therapy - one cohort assigned to continue anticoagulation indefinitely with direct oral anticoagulants, and another assigned to discontinue anticoagulation indefinitely. The model adopted a cycle length of 1 month and a lifetime horizon. The economic analysis adopted a third-party payer perspective relating to the Canadian publicly-funded healthcare system. The long-term risks and case-fatality rates of recurrent VTE and major bleeding, with and without extended anticoagulation, were sourced from our recently published systematic reviews (Khan F, BMJ 2019;Khan F, Ann Intern Med 2021). Additional data related to transition probabilities, costs, and utility values were obtained from highest quality published sources identified through a targeted literature search. Future costs and QALYs were discounted at an annual rate of 1.5% as per Canadian guidelines. The model structure, input parameters, and assumptions were validated by clinical experts to ensure that they coincided with current clinical practice.
Results: In a hypothetical cohort of 1000 patients, continuing anticoagulation indefinitely, compared to discontinuing anticoagulation, prevented 253 recurrent VTE events (number needed to treat = 4) and induced an additional 69 major bleeding events (number needed to harm = 15). Indefinite anticoagulation resulted in higher health system costs ($70,019.35 vs. $61,438.10 per person) and no improvement in QALYs (15.26 vs. 15.31 per person; incremental difference of -0.05 QALYs or -18.25 quality adjusted life-days) [Table 1]. Model results were most sensitive to the annual risk of major bleeding and case-fatality rate of major bleeding during extended anticoagulation however, in all one-way sensitivity analyses, discontinuing anticoagulation remained economically dominant (i.e., lower costs and similar QALYs) over continuing anticoagulation indefinitely, at a willingness-to-pay (WTP) threshold of Can$50,000 per QALY. In probabilistic analyses, the probability of indefinite anticoagulation being the cost-effective treatment strategy was 0% at a WTP threshold of Can$50,000 or Can$100,000 per QALY.
Conclusions: Indefinite anticoagulation for a first unprovoked VTE is unlikely to either result in a net clinical benefit or be cost-effective. With no net gain in QALYs (albeit a small net loss), there is no rationale for continuing anticoagulation indefinitely in all (i.e., unselected) patients with a first unprovoked VTE. However, the clinical and cost-effectiveness of indefinite anticoagulation in subgroups of patients at high risk of recurrent VTE and low risk of major bleeding requires further investigation, and will be an important next step.
Disclosures
No relevant conflicts of interest to declare.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract
Asterisk with author names denotes non-ASH members.